If you’re a veteran trying to access healthcare — or a provider trying to get paid — dealing with the VA Office of Community Care can feel like running an obstacle course blindfolded. The Office of Integrated Veteran Care (IVC) was established to enhance collaboration and streamline access to care for Veterans by combining existing offices, handling billing activities, and improving coordination amidst the challenges posed by an increasing reliance on community care providers.
This guide will show you how to cut through the red tape, avoid common pitfalls, and use the VA Community Care Network to get the care or payments you deserve.
What Is the VA Community Care Network?
The VA Community Care Network (CCN) was created by the Department of Veterans Affairs to connect eligible veterans with community providers when VA facilities cannot deliver the health care services needed in a timely or convenient way.
Third-party administrators (TPAs) like Optum Serve and TriWest manage the networks, covering veterans from North Dakota to Puerto Rico and the Virgin Islands.
The goal is timely, high-quality care that adheres to quality standards — without months-long waits or hours of travel, thereby improving veterans access to essential health care services.
The reality is you must know how the system works to make it work for you.
Who Qualifies for VA Community Care?
You may be eligible if:
- You are enrolled in VA health care
- You face long wait times (over 20–28 days)
- You live far from a VA facility (more than 30–60 minutes)
- The VA does not offer the specific care needed
- It is in your best medical interest to go outside
Veterans can access various types of medical care through the program, including specialized treatments, routine check-ups, and emergency services.
Pro Tip: Always ask for a Community Care referral if your VA doctor suggests a service not available at your facility. Push back if needed — it is your legal right under the MISSION Act.
Receiving Care in the Community
Receiving care in the community through the VA Community Care Network (CCN) offers eligible veterans a convenient and flexible way to access high-quality health care services. The CCN is a network of community providers who have partnered with the Department of Veterans Affairs (VA) to provide care to veterans outside of VA facilities.
To receive care in the community, veterans must meet specific eligibility requirements, which are determined on a case-by-case basis by VA healthcare providers. Eligible veterans can choose from a network of community providers who have contracted with the VA to provide care.
Community care providers offer a range of health care services, including primary care, specialty care, mental health services, and nursing homes. Veterans can access community care through their local VA medical facility or by contacting the VA directly.
The VA Community Care Network is designed to improve care coordination and provide veterans with access to high-quality, timely care in their local communities. Community care is an essential part of the VA’s mission to provide veterans with access to quality health care.
How to Find Community Providers
Veterans can find community providers by:
- Searching the VA Community Care Directory
- Contacting their VA medical center’s community care office
- Reaching out through the third-party administrators (Optum Serve or TriWest)
Warning:
Not every listed provider actively accepts new veteran patients. Always call first to confirm.
Community Care Providers and the VA
Community care providers play a critical role in the VA’s community care program. These providers are healthcare professionals who have contracted with the VA to provide care to veterans outside of VA facilities.
To become a community care provider, healthcare professionals must meet specific requirements, including being licensed and certified in their field. They must also agree to abide by the VA’s standards for quality and safety.
The VA works closely with community care providers to ensure that veterans receive high-quality care. The VA provides community care providers with training and support to help them deliver care that meets the unique needs of veterans.
Community care providers are an essential part of the VA’s community care program, and the VA is committed to working with them to provide high-quality care to eligible veterans.
How Care Coordination Should Work (And Often Does Not)
Ideally, your VA team and your community provider should coordinate:
- Referrals
- Medical records
- Billing paperwork
In reality, coordination often breaks down. Poor communication can mean:
- Missed appointments
- Duplicated tests
- Billing disasters
- Care delays
Pro Tip:
Keep your own copies of referrals and medical records. Assume you will need to oversee your own care path between VA and the provider.
Provider Billing and Payment Basics
If you are a community care provider, here is how to avoid payment delays:
- Verify veteran eligibility and authorization before delivering care
- Use the correct referral number when billing
- Submit complete documentation (progress notes, procedure codes, etc.)
- Bill electronically through your TPA portal (Optum Serve, TriWest)
- Monitor claim status weekly through the portal
What to Do If You Are Not Getting Paid
If payments are delayed or denied:
- Contact the TPA first (Optum Serve or TriWest)
- Use their provider support team to troubleshoot
- Escalate unresolved issues through the VA Provider Payments portal
- Document everything: names, dates, promises
- Push politely but persistently until you get paid
Pro Tip:
The providers who escalate early and document everything tend to get paid faster.
Technology and Innovation: Making Things Better (Slowly)
The VA is upgrading technology across community care:
- Telehealth expansions now allow veterans to see doctors remotely
- Electronic Health Record (EHR) integration improves data-sharing
- Predictive modeling flags claims likely to be denied for faster fixes
- Mobile tools allow providers to track payments and manage claims easily
Caution:
Not all offices are fully up to speed yet. Always double-check referrals, records, and billing.
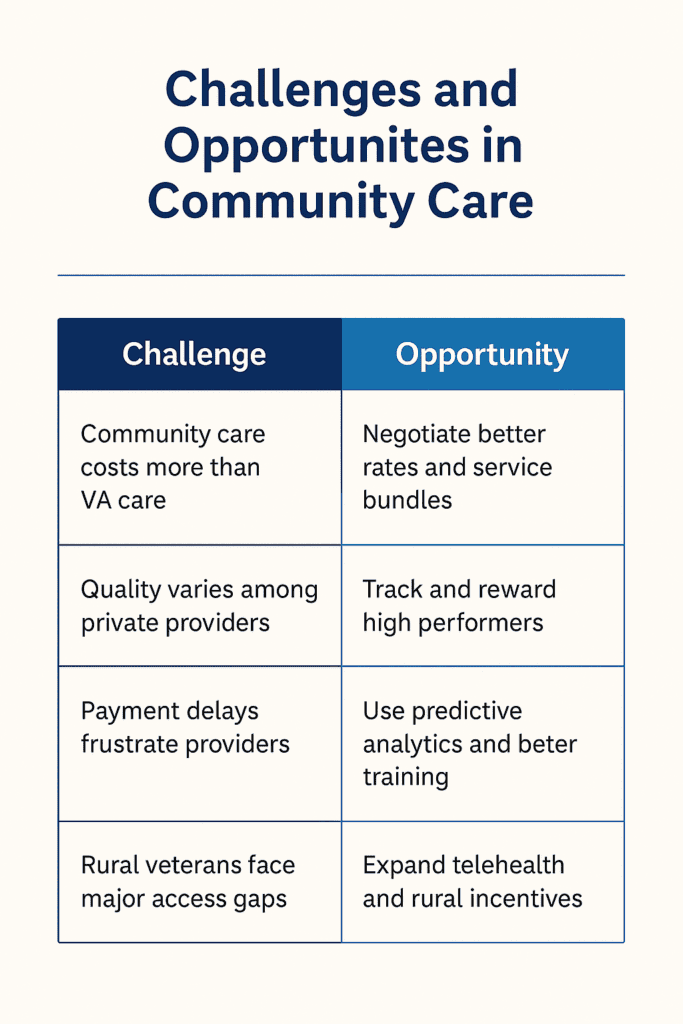
Challenges and Opportunities in Community Care
| Challenge | Opportunity |
|---|---|
| Community care costs more than VA care | Negotiate better rates and service bundles |
| Quality varies among private providers | Track and reward high performers |
| Payment delays frustrate providers | Use predictive analytics and better training |
| Rural veterans face major access gaps | Expand telehealth and rural incentives |
Despite the growing pains, the Community Care Network provides vital options — especially for veterans living in rural or underserved areas.
Challenges and Opportunities Infographic
Additional Resources
The VA offers a range of additional resources to help veterans navigate the community care program. These resources include:
- The VA Community Care Network website, which provides information on community care providers and how to access care in the community.
- The VA’s toll-free hotline, which provides veterans with information and assistance on community care.
- The VA’s online portal, which allows veterans to access their medical records and communicate with their healthcare providers.
- The VA’s community care coordinators, who work with veterans to coordinate their care and ensure that they receive the services they need.
The VA is committed to providing veterans with access to high-quality health care services, and the community care program is an essential part of this effort. By working with community care providers and providing additional resources, the VA is able to offer veterans a range of options for receiving care in the community.
Conclusion
The VA Office of Community Care The VA Office of Community Care was built to give veterans in the district of columbia more options.
But to actually benefit, you must understand the system, stay proactive, and protect yourself.
Whether you are a veteran fighting for your referral or a provider chasing a payment, DisabledVeterans.org is here to arm you with the knowledge you need.
Use this guide. Ask questions. Escalate when necessary.
The system will not advocate for you — but we will.
Final Checklist
For Veterans:
- Confirm eligibility
- Demand your referral
- Choose and confirm your provider
- Manage your own records
For Providers:
- Verify referrals
- Submit clean claims
- Track claims weekly
- Escalate problems early
Call to Action
Need More Help?
Visit VA’s Community Care Hub or contact your VA patient advocate today.